Obesity is becoming a global epidemic, with harmful health, psychosocial and economic effects(Reference James, Leach, Kalamara and Shayeghi1, Reference Must, Spadano, Coakley, Field, Colditz and Dietz2). Actions focusing on reducing the prevalence and incidence of obesity and weight gain should constitute a public health priority. Weight gain is associated with increased risk of diabetes, hyperinsulinaemia, insulin resistance, hyperlipidaemia and hypertension(Reference Wannamethee and Shaper3–Reference Norman, Bild, Lewis, Liu and West8). Several studies have been conducted in order to identify predisposing factors associated with the incidence of weight gain. The existing literature suggests that younger adults, women and African Americans are at higher risk of gaining weight over time and becoming overweight(Reference Williamson9–Reference Sheehan, DuBrava, DeChello and Fang17). Still, the evidence is not conclusive; there are equivocal findings(Reference Sheehan, DuBrava, DeChello and Fang17, Reference Vasan, Pencina, Cobain, Freiberg and D’Agostino18) and the results may be affected by confounding parameters, such as socio-economic and marital status, changes in smoking habits and physical activity patterns, or inherent sample characteristics and longitudinal changes(Reference Brown, Williams, Ford, Ball and Dobson19–Reference Kahn, Williamson and Stevens22). Furthermore, potential ‘protective’ dietary components contributing to weight maintenance and prevention of weight gain have been identified, i.e. fibre intake(Reference Ludwig, Pereira, Kroenke, Hilner, Van Horn, Slattery and Jacobs23), breakfast cereals consumption(Reference Bazzano, Song, Bubes, Good, Manson and Liu24, Reference Schulz, Kroke, Liese, Hoffmann, Bergmann and Boeing25), vegetable intake(Reference Kahn, Tatham, Rodriguez, Calle, Thun and Heath26) and adherence to the Mediterranean diet(Reference Mendez, Popkin and Jakszyn27). Conversely, increased consumption of meat, French fries, dairy products and sweets has been associated with short- or long-term risk for weight gain(Reference Schulz, Kroke, Liese, Hoffmann, Bergmann and Boeing25, Reference Kahn, Tatham, Rodriguez, Calle, Thun and Heath26, Reference French, Jeffery, Forster, McGovern, Kelder and Baxter28).
Prospective studies on weight changes and incidence of obesity in population samples in the Mediterranean area are scarce. In the present study we investigated the 5-year incidence and determinants of overweight/obesity, as well as weight gain, in a random sample of CVD-free adults from the ATTICA epidemiological study(Reference Pitsavos, Panagiotakos, Chrysohoou and Stefanadis29), where a high prevalence of obesity was reported at the baseline evaluation(Reference Panagiotakos, Pitsavos, Chrysohoou, Risvas, Kontogianni, Zampelas and Stefanadis30).
Methods
Study design
The ATTICA study, a health and nutrition survey, was conducted in the province of Attica (including 78 % urban and 22 % rural areas), Greece, during 2001 to 2002(Reference Pitsavos, Panagiotakos, Chrysohoou and Stefanadis29). The sampling anticipated including only one participant per household; it was random, multistage and based on the age and sex distribution of the province of Attica provided by the National Statistical Service (census of 2001). People living in institutions were excluded from the sampling. From May 2001 to December 2002, 4056 inhabitants from the above area were randomly selected for enrolment into the study. Of them, 3042 agreed to participate (75 % participation rate); 1514 of the participants were men and 1528 were women. The selected sample can be considered representative because there were only minor, insignificant differences in sex and age distribution between the study population and the target population. All participants were interviewed by trained personnel (cardiologists, other physicians, dietitians and nurses) on the basis of a standard questionnaire.
Baseline measurements
At baseline, participants’ demographic characteristics (age, sex, mean annual income and years of schooling as a proxy for social status), detailed medical history, dietary and other lifestyle habits (such as smoking and habitual/leisure-time physical activity) were evaluated. Food consumption was evaluated using the EPIC–Greece questionnaire, a validated semi-quantitative FFQ developed for the Greek cohort of the European Prospective Investigation into Cancer and Nutrition(Reference Katsouyanni, Rimm, Gnardellis, Trichopoulos, Polychronopoulos and Trichopoulou31). In particular, all participants were asked to report the average intake (per week or day) of several food items that they consumed during the last 12 months. Then, the frequency of consumption was quantified approximately in terms of the number of times a month a food was consumed. Alcohol consumption was measured in wine glasses (100 ml) and quantified by ethanol intake (grams per drink). In order to describe overall dietary patterns, a composite score was used; specifically, a special Mediterranean diet score was applied (range 0–55) based on the rationale of the Mediterranean dietary pyramid(Reference Panagiotakos, Pitsavos and Stefanadis32). Energy intake was assessed using food composition tables(Reference Trichopoulou and Georga33). Furthermore, the degree of low energy reporting was evaluated by using the ratio of energy intake (EI) to BMR(Reference Goldberg, Black, Jebb, Cole, Murgatroyd, Coward and Prentice34), as described elsewhere(Reference Yannakoulia, Panagiotakos, Pitsavos, Bathrellou, Chrysohoou, Skoumas and Stefanadis35). Participants with EI:BMR < 1·14 were classified as ‘energy under-reporters’ or ‘low energy reporters’.
Smokers were defined as those who were smoking at least one cigarette daily during the past year or had recently stopped smoking (during a year); the rest of the participants were defined as non-smokers. For the ascertainment of physical activity status, the IPAQ (International Physical Activity Questionnaire) was used as an index of weekly energy expenditure, using frequency (times per week), duration (in minutes per time) and intensity of sports or other habits related to physical activity (in expended energy per time). Participants who did not report any physical activities were defined as physically inactive (sedentary lifestyle).
Arterial blood pressure was measured three times at the right arm at the end of the physical examination, with subject in sitting position at least for 30 min. Patients whose average blood pressure levels were ≥140/90 mmHg or who were under antihypertensive medication were classified as having hypertension(Reference Chobanian, Bakris and Black36). In addition, for classification purposes, hypercholesterolaemia was defined as serum total cholesterol level >200 mg/dl or the use of lipid-lowering agents(37) and diabetes mellitus as fasting blood glucose level >125 mg/dl or the use of antidiabetic medications(38).
Height was measured to the nearest 0·5 cm, without shoes, and weight to the nearest 100 g, without shoes, in light undergarments. BMI was calculated as weight (in kilograms) divided by the square of height (in metres). In accordance with the WHO recommendation(39), overweight was defined as BMI between 25·0 and 29·9 kg/m2, while obesity as was defined as BMI ≥ 30·0 kg/m2.
The anxious state was assessed using the Spielberger State-Trait Anxiety Inventory (STAI), a twenty-item self-reported questionnaire. The STAI differentiates between the temporary condition of ‘state anxiety’ and the more general and long-standing quality of ‘trait anxiety’(Reference Spielberger, Gorsuch and Lushene40, Reference Anisman and Merali41). The twenty items were rated from 1 to 4 in terms of frequency categories (never; sometimes; often; always) and total scores were obtained by summing the values assigned to each response (range from 20 to 80). Higher scores indicate more trait or state anxiety(Reference Spielberger, Gorsuch and Lushene40). In the present study, the Greek version of the instrument was used(Reference Fountoulakis, Papadopoulou, Kleanthous, Papadopoulou, Bizeli, Nimatoudis, Iacovides and Kaprinis42). Depressive symptomatology was assessed through a translated version of the Zung Self-Rating Depression Scale (ZSDS), a well-known self-rating scale used worldwide for the measurement of depression(Reference Zung43). The ZSDS consists of twenty items that cover affective, psychological and somatic symptoms (range from 20 to 80). Higher scores on this scale are indicative of more severe depression.
Follow-up
During 2006, the ATTICA study investigators performed the 5-year follow-up of the participants. Of the 3042 initially enrolled participants, vital status was obtained from 1044 men and 1057 women (69 % participation rate). Of them, thirty-two (2·1 %) men and twenty-two (1·4 %) women had died during the 5-year period. Of the participants who did not participate in the re-examination, 25 % were not found because of missing or wrong addresses and telephone numbers and 5 % refused to be re-examined. Participants who were lost to follow-up were more frequently smokers (P < 0·001) and less physically active (P = 0·03) at the baseline examination compared with those who were followed up. No significant differences were observed between those who were lost at follow-up and the rest of the participants regarding sex (P = 0·99), baseline age (P = 0·78), education level in years of schooling (P = 0·67), as well as the presence of hypertension (P = 0·12), diabetes (P = 0·27) and hypercholesterolaemia (P = 0·12).
The re-examination was based on telephone interviews (80 % of the participants) and on face-to-face interviews when a telephone number was not available. The re-examination included self-reported information on vital status (death from any cause or due to CVD), development of CHD or other metabolic conditions among people who did not have these disorders at baseline, body weight and height, and changes in lifestyle habits including dietary intake. For the present analysis, individuals who reported significant dietary changes due to various reasons during the 5-year follow-up period (n 290), as well as those who did not answer this question about dietary changes during the preceding 5 years (n 184), were excluded. Moreover, 209 participants reported in the baseline examination that they were on a slimming diet. These participants were also excluded from the present analysis. Furthermore, taking into account those who were lost to follow-up, those who died during the 5-year period and those who were excluded because of the aforementioned reasons, data from 1364 participants are analysed in the present work.
Weight change was used to categorize subjects as weight-stable (those not changing their weight by >3 kg in the 5-year period), weight losers (those who decreased their weight by >3 kg) and weight gainers (those who increased their weight by >3 kg). The threshold of 3 kg for the definition of weight maintenance was based on both statistical and biological bases: it is equivalent to 25 % of the standard deviation of mean body weight of our participants and ensures that an adequate sample is included in the group of weight-stable participants. Furthermore, it represents approximately 4 % of the initial body weight or 0·6 kg/year, a value that is within the range of values used in studies with prior weight change avoided or unspecified(Reference Stevens, Truesdale, McClain and Cai44).
Statistical analysis
Continuous variables are presented as mean values with their standard deviation, and categorical variables as absolute and relative frequencies. Associations between categorical variables were tested using the χ 2 test. Comparisons of mean values of normally distributed continuous variables between those who lost weight, gained weight or remained weight-stable (±0·25 sd from baseline BMI or ±3 kg) were performed using ANOVA, after controlling for equality of variances using Levene’s test. The likelihood for the development of obesity (dependent outcome) during the 5-year period, according to the participants’ baseline sociodemographic, lifestyle and clinical characteristics (independent factors), was estimated using odds ratios and their corresponding 95 % confidence intervals through multiple logistic regression analyses. Interactions between sex and other covariates were tested in all steps and, when they were significant, remained in the final model. Deviance residuals were used to evaluate the model’s goodness-of-fit, and the −2 log likelihood of the initial and final model were also calculated. All reported P values are based on two-sided tests and compared with a significance level of 5 %. The Statistical Package for Social Sciences statistical software package version 14 (SPSS Inc., Chicago, IL, USA) was used for all statistical calculations.
Results
During the 5-year follow-up period, 9·8 % of men and 7·2 % of women participants who were normal-weight at the baseline examination developed obesity (n 47), while 32·7 % of men and 28·2 % of women who were overweight at baseline developed obesity (n 105). Thus, the overall 5-year incidence of obesity was 21·8 % in men and 11·9 % in women. The ratio of men to women demonstrated that more men than women developed obesity, while more women than men became overweight; no gender differences were observed regarding the 5-year incidence of overweight or obesity (P = 0·10). Table 1 illustrates the 5-year incidence of overweight or obesity among study participants who were classified as normal-weight at the baseline examination. Middle-aged individuals were more likely to develop obesity during the follow-up period compared with younger or older adults (P < 0·001). Furthermore, 25·7 % of males and 30·8 % of females who were obese at baseline remained obese at the 5-year follow-up examination.
Table 1 Five-year incidence of overweight and obesity among ATTICA study participants classified as normal-weight at the baseline examination
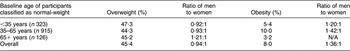
N/A, not applicable.
During the 5-year period, BMI in men decreased on average by 0·40 (sd 0·49) kg/m2, whereas in women it decreased by 0·46 (sd 0·49) kg/m2 (P for gender difference = 0·05). When the analysis was stratified by baseline obesity status, it was revealed that, among initially normal-weight participants, the mean change in BMI was 2·1 (sd 3·1) kg/m2 in men (i.e. weight gain, P < 0·001) and 3·1 (sd 3·2) kg/m2 in women (i.e. weight gain, P < 0·001) (P for gender difference = 0·98), whereas among initially overweight participants the mean change in BMI was −0·85 (sd 3·8) kg/m2 in men (i.e. weight loss, P < 0·001) and −0·78 (sd 3·8) kg/m2 in women (i.e. weight loss, P = 0·003) (P for gender difference = 0·72). Similar results were observed among participants classified as obese at baseline; the mean change in BMI was −4·0 (sd 3·1) kg/m2 in men (i.e. weight loss, P < 0·001) and −3·7 (sd 3·1) kg/m2 in women (i.e. weight loss, P < 0·001) (P for gender difference = 0·80).
Two hundred and twelve subjects were classified as weight-stable, 623 as weight losers and 529 as weight gainers. Associations of BMI change group (stable weight; weight loss; weight gain) at 5-year follow-up with several sociodemographic, lifestyle, dietary and psychological characteristics are presented in Table 2. Unadjusted analysis showed that compared with those who remained stable, weight losers were more likely to be older, men, obese, with abnormal waist circumference and hypertensive, and had lower adherence to the Mediterranean diet. Moreover, those who gained weight were more likely to be younger, more educated, and less frequently to be obese and/or diabetic (Table 2). It is of interest that those who gained weight were closer to the Mediterranean dietary pattern; however, this association became insignificant in the multivariate analysis, when the EI:BMR ratio was taken into account.
Table 2 Results of analyses that evaluated the association between sociodemographic, lifestyle, biological and clinical factors (independent) by group of BMI change in the ATTICA study participants (n 1364)
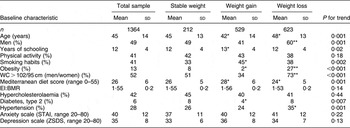
WC, waist circumference; EI, energy intake; STAI, Spielberger State-Trait Anxiety Inventory; ZSDS, Zung Self-Rating Depression Scale.
*P < 0·05, **P < 0·01: Bonferroni-corrected P value for the comparison between the weight gain or weight loss group and those who remained weight-stable during the follow-up period.
With regard to the incidence of obesity, multiple logistic regression analysis was applied to evaluate the 5-year incidence of obesity among those who were normal-weight or overweight at baseline examination. It was revealed that men were 1·62 times more likely to develop obesity compared with women; abnormal waist circumference increased the risk for obesity 2·01-fold, smoking habits increased the aforementioned risk 1·50-fold, and the presence of hypercholesterolaemia at baseline increased the risk for developing obesity 1·60-fold, irrespective of age, physical activity, dietary habits and other baseline characteristics of the participants (Table 3). Furthermore, LDL cholesterol levels were associated with obesity incidence, since a 10 mg/dl difference in baseline levels was associated with 4·6 % higher likelihood of being obese (OR = 1·01, 95 % CI 1·00, 1·02, P = 0.001). On the contrary, TAG levels were not associated with the development of obesity (OR = 1·00, 95 % CI 0·00, 1·01, P = 0.16); similarly, HDL cholesterol levels were not associated with obesity status at follow-up (OR = 0·99, 95 % CI 0·97, 1·00, P = 0·32).
Table 3 Results from multiple logistic regression analyses that evaluated sociodemographic, lifestyle, biological and clinical baseline characteristics in relation to 5-year incidence of obesity in the ATTICA study participants (n 1364)
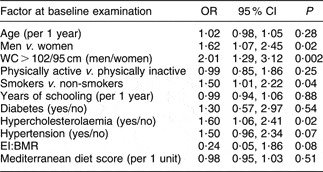
WC, waist circumference; EI, energy intake.
Discussion
In the present work the incidence rate of obesity over 5 years was evaluated in a population-based sample of free-living adults. The 5-year incidence of overweight and obesity among volunteers who were classified as normal-weight at baseline examination was 45·4 % and 8·0 %, respectively; in other words, more than one out of two Greek adults of the ATTICA study developed excess body weight in 5 years. These values are among the highest reported in the literature(Reference Ball, Crawford, Ireland and Hodge10, Reference McTigue, Garrett and Popkin16, Reference Vasan, Pencina, Cobain, Freiberg and D’Agostino18, Reference Williamson, Kahn, Remington and Anda45) and the study the first that prospectively examined weight gain and obesity in the Greek population. Ball et al.(Reference Ball, Crawford, Ireland and Hodge10) also recorded a high percentage (11·2 %) of Greek-origin study participants becoming obese in a large multi-ethnic cohort of men and women in Australia, but owing to the nature of the investigation the authors could not presume the contribution of ethnicity or acculturation in their results. In another Mediterranean country, Spain, 7·9 % and 6·9 % of initially overweight women and men respectively became obese, whereas 13·8 % and 23·0 % of initially normal-weight women and men respectively became overweight, during a 3-year follow-up period according to information collected from the EPIC–Spain cohort(Reference Mendez, Popkin and Jakszyn27). Hence, our findings indicate that obesity remains a serious health problem for the Greek population; the alarming rates of excess body weight continue to increase and thus so too does the incidence of weight gain-related metabolic problems.
In the multivariate analysis men were at higher risk to develop obesity during the 5-year follow-up period, a finding which is consistent with the higher prevalence of obesity among men at baseline(Reference Panagiotakos, Pitsavos, Chrysohoou, Risvas, Kontogianni, Zampelas and Stefanadis30). Dieting is commonly practised among adolescent girls in Greece(Reference Yannakoulia, Karayiannis, Terzidou, Kokkevi and Sidossis46) and we may hypothesize that the interest in slimming may also continue during adulthood, thus explaining, at least in part, the lower incidence of obesity in female study participants despite the higher incidence of overweight. Furthermore, initially normal-weight and overweight participants with central obesity at baseline, as well as with hypercholesterolaemia and smoking, were more prone to become obese. Regardless of educational status, the obesity epidemic disproportionately affects those at cardiovascular risk to become obese and consequently increases their higher risk. Their unfavourable metabolic profile did not prevent them from worsening their health status, despite the recommendations for a healthy lifestyle that had probably been received from health professionals. Changing dietary and physical activity habits is not an easy task. The adoption of a healthy diet and the attainment of energy balance require a series of behavioural adjustments in eating patterns with regard to meal planning, food selection, food preparation, dining out and portion control, as well as appropriate responses to eating challenges. Similar changes are also required for increasing lifestyle physical activity. It has been suggested that people with risk factors for chronic diseases receive a great amount of information, often confusing and contradictory, from a variety of sources, without respective attention to behavioural changes and the collaborative aspect of intervention, factors that predispose them to low adherence to lifestyle recommendations(Reference Yannakoulia47), as was evident from the results of the present study.
Adoption of the Mediterranean diet has been associated with favourable effects on lipoprotein levels, endothelium function, insulin resistance and metabolic syndrome(Reference Serra-Majem, Roman and Estruch48). With regard to body weight and obesity status, some investigators have shown that a Mediterranean dietary pattern was inversely related to BMI(Reference Panagiotakos, Chrysohoou, Pitsavos and Stefanadis49, Reference Schroder, Marrugat, Vila, Covas and Elosua50) whereas others did not find any association(Reference Trichopoulou, Naska, Orfanos and Trichopoulos51). Prospectively, the findings are also equivocal. High (but not moderate) adherence to a Mediterranean diet was associated with reduced incidence of obesity in a Spanish population(Reference Mendez, Popkin and Jakszyn27). In contrast, the dose–response relationship between weight gain and adherence to a Mediterranean dietary pattern observed in the SUN cohort (again a Spanish population sample) became non-significant after adjusting for potential confounders; the same was evident when the change in adherence to the Mediterranean diet was used(Reference Sanchez-Villegas, Bes-Rastrollo, Martinez-Gonzalez and Serra-Majem52). Consistent with the latter work, our analysis did not show an association between the Mediterranean diet score and 5-year incidence of obesity in the multivariate analysis, when confounding factors, including low energy reporting, were taken account. Consequently, the results of the ATTICA study suggest that, even if the Mediterranean dietary pattern has an impact on body weight at a cross-sectional level(Reference Panagiotakos, Chrysohoou, Pitsavos and Stefanadis49), it does not significantly explain 5-year body weight changes. Previous studies also failed to provide significant associations between dietary factors, either at a nutrient or at a dietary pattern level, with subsequent BMI changes or obesity incidence(Reference Colditz, Willett, Stampfer, London, Segal and Speizer11, Reference Togo, Osler, Sorensen and Heitmann53, Reference Jorgensen, Sorensen, Schroll and Larsen54). Colditz et al.(Reference Colditz, Willett, Stampfer, London, Segal and Speizer11) argued that other factors, like age and prior weight loss, were far stronger predictors of weight change than intakes of specific nutrients. Furthermore, due to the nature of the present study, we evaluated obesity incidence only in those participants reporting that their diet remained unchanged during the 5-year follow-up period. One may speculate that changes in dietary patterns would predict changes in anthropometric variables, as previously shown(Reference Newby, Weismayer, Akesson, Tucker and Wolk55), but once a dietary pattern is established this does not account for further weight changes. Finally, several methodological issues have arisen in the literature regarding the use of Mediterranean scores. Inclusion of lipid intake in the score or scoring of dairy products and nuts have been proposed as methodological concerns regarding the association between adherence to a Mediterranean diet and obesity(Reference Trichopoulou, Naska, Orfanos and Trichopoulos51, Reference Sanchez-Villegas, Bes-Rastrollo, Martinez-Gonzalez and Serra-Majem52).
The present observational study has some limitations. The baseline evaluation was performed once and may be prone to measurement error; another drawback is the use of self-reported weight and height at follow-up. Although the validity of self-reported anthropometric data has been questioned(Reference Yannakoulia, Panagiotakos, Pitsavos and Stefanadis56–Reference Nyholm, Gullberg, Merlo, Lundqvist-Persson, Rastam and Lindblad58), our methodology is similar to those of other cross-sectional surveys and follow-up epidemiological studies in Europe, the USA and Australia(Reference Wannamethee and Shaper3, Reference Ball, Crawford, Ireland and Hodge10, Reference Colditz, Willett, Stampfer, London, Segal and Speizer11, Reference Sheehan, DuBrava, DeChello and Fang17, Reference Kahn, Tatham, Rodriguez, Calle, Thun and Heath26, Reference Mendez, Popkin and Jakszyn27, Reference Sanchez-Villegas, Bes-Rastrollo, Martinez-Gonzalez and Serra-Majem52) and therefore the results are comparable. We paid special attention to include in the analysis only subjects who had stable dietary habits at baseline and also those who firmly reported no change in their diet during the follow-up period. On the other hand, despite the high correlation coefficients between measured and self-reported anthropometric data and the moderate level of agreement between the distributions of self-reported and measured obesity status groups that we have previously found in this population at the baseline assessment(Reference Yannakoulia, Panagiotakos, Pitsavos and Stefanadis56), we believe that the study possibly provides a conservative estimate of the obesity incidence and that the rates would be higher if information on measured weight was available at follow-up. Another limitation of the study was the response rate of 69 % at follow-up. Participation in epidemiological studies has been declining generally(Reference Morton, Cahill and Hartge59); however, our retention rate was among the lowest reported in the literature(Reference Wannamethee and Shaper3, Reference Ball, Crawford, Ireland and Hodge10, Reference Lewis, Jacobs, McCreath, Kiefe, Schreiner, Smith and Williams13, Reference Mendez, Popkin and Jakszyn27, Reference Sanchez-Villegas, Bes-Rastrollo, Martinez-Gonzalez and Serra-Majem52, Reference Newby, Weismayer, Akesson, Tucker and Wolk55). Moreover, we observed that participants who were lost to follow-up were more frequently smokers and sedentary at the baseline examination. These findings may bias the final model that evaluated predictors of obesity, since physical inactivity has been reported as a prognostic marker of obesity in some studies. Although this bias may have mediated the lack of significant association between physical activity status and incidence of obesity in our sample, we cannot entirely answer this question from our analysis.
In conclusion, the findings of the 5-year follow-up of the ATTICA study indicate high rates of overweight and obesity incidence in the Greek population. We revealed that initially normal-weight subjects with an unfavourable metabolic profile at baseline were at higher risk for developing obesity prospectively. Preventive measures for excess body weight should be urgently addressed in Greece, with high priority on those with metabolic risk factors.
Acknowledgements
Authors’ contributions and conflict of interest: M.Y. had the concept of the paper, interpreted the results and wrote the paper; D.P. designed the study, supervised the sampling, performed data analysis and wrote the paper; C.P., C.C. and I.S. designed the study, supervised data collection and critically reviewed the paper; Y.L. supervised the follow-up; C.S. supervised the study and critically reviewed the paper. All authors contributed to the final manuscript and none declared any conflict of interest.
Sources of funding: The ATTICA study is supported by research grants from the Hellenic Cardiological Society (HCS2002) and the Hellenic Atherosclerosis Society (HAS2003).
Acknowledgements: The authors would like to thank the field investigators of the ATTICA study: Ioanna Papaioannou, Natassa Katinioti, Akis Zeimbekis, Dina Masoura, Labros Papadimitriou and Spiros Vellas, for their assistance in the physical examination; Charalabos Papageorgiou and Efi Tsetsekou for their assistance in the psychological evaluation; the laboratory team: George Dedousis, Carmen Vassiliadou (genetic analysis), Manolis Kambaxis and Konstadina Palliou, for the nutritional evaluation; Marina Toutouza-Giotsa, Constadina Tselika and Sia Poulopoulou for the biochemical evaluation; and Maria Toutouza for the database management.







